Elbow
Care and Management
Arthroscopic Debridement of the Elbow
During this outpatient procedure, the surgeon examines the inside of the elbow joint with a camera called an arthroscope. The surgeon identifies and corrects problems with the bones, ligaments and tendons of the elbow.
Aspiration of the Olecranon Bursa
This outpatient procedure relieves pain and swelling in the elbow caused by bursitis, or inflammation of the bursa. The bursa is a fluid-filled sac between the skin and bones of the elbow.
Cubital Tunnel Release
This surgery treats cubital tunnel syndrome. That’s a compression or irritation of the ulnar nerve at the elbow. During this surgery, the nerve is given more room.
Medial Epicondylectomy
This outpatient procedure, performed under general or regional anesthesia, removes the medial epicondyle (the bony bump on the inner side of the elbow) to alleviate compression of the ulnar nerve. Medial epicondylectomy is used to treat cubital tunnel syndrome.
Medial Ulnar Collateral Ligament Reconstruction (Tommy John Surgery)
This procedure is designed to repair a torn elbow ligament – an injury typically caused by strong, repetitive overhead throwing motions of the arm or by dislocation of the elbow. It was first performed in 1974 on baseball pitcher Tommy John.
Conditions
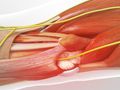
Biceps Tendonitis (at the Elbow)
This is a problem with a tendon in your elbow. It’s called the “distal biceps tendon.” It connects the biceps muscle of your upper arm to the radius bone at the elbow. With this condition, the tendon becomes painfully inflamed or irritated.
Cubital Tunnel Syndrome
This condition, also called “ulnar nerve entrapment,” happens to the ulnar nerve in your elbow. This nerve travels along the inner side of your elbow and down to your hand. It’s the nerve that makes the jolt you feel when you bump your “funny bone.” With this condition, your ulnar nerve is compressed, stretched or irritated.
Elbow Bursitis
This is a swelling of a fluid-filled sac in the back of your elbow. This sac is called the “olecranon bursa.” You have similar sacs near other large joints throughout your body. They act as cushions between your bones and your soft tissues. Normally they have a small amount of fluid inside them. But sometimes they can swell. That is called “bursitis.”
Hyperextension Injury of the Elbow
This happens when you extend your elbow back farther than it’s supposed to go. That damages the bones and soft tissues in your joint. Hyperextension can dislocate or even fracture your elbow.
Lateral Epicondylitis (Tennis Elbow)
This condition, commonly called tennis elbow, is an inflammation of the tendons that connect the muscles of the forearm to the elbow. The pain is primarily felt at the lateral epicondyle, the bony bump on the outer side of the elbow.
Medial Epicondylitis (Golfer’s Elbow)
This condition, commonly called golfer’s elbow, is an inflammation of the tendons that connect the muscles of the forearm to the elbow. The pain is primarily felt at the medial epicondyle, the bony bump on the inner side of the elbow.
Osteochondritis Dissecans of the Elbow
This is a disorder that most often affects young athletes. It happens when part of a bone in the elbow loses its blood supply. It weakens, and so does the cartilage that covers it. Bone and cartilage may break off and drift around in the elbow. That can cause the joint to catch and lock up.
Overuse Injuries of the Elbow
If you are an athlete, or if you work with your arms and hands, your elbows may be at risk for an overuse injury. This is an injury caused by repetitive motions. This type of injury can be a problem for people who play sports such as tennis or baseball. Children also have a higher risk, because their bones are still growing.
Throwing Injuries of the Elbow
Throwing overhand again and again puts a lot of stress on your elbow. It can lead to injury. Young athletes, in particular, are at risk. Some play sports all year without learning how to throw properly. And, their bones are still growing. Let’s look at how the elbow can be damaged.
Triceps Tendonitis
This is an inflammation of a tendon at the back of your elbow. It’s called the “triceps” tendon. It anchors your upper arm’s triceps muscle to the ulna (one of the bones of your forearm).
Ulnar Collateral Ligament Injury
Like other joints, the elbow is held together by strong bands of tissue called “ligaments.” On the elbow’s inner side is the ulnar collateral ligament complex. We call it the “UCL.” It’s made of three bands that connect the humerus (the upper arm bone) to the lower arm’s ulna. The UCL is the elbow ligament most often injured by baseball pitchers and by other athletes who play throwing sports.
Foot, Ankle and Lower Leg
Care and Management
Achilles Tendon Lengthening
This procedure is designed to treat problems with the Achilles tendon, such as chronic tendonitis or a short or contracted Achilles tendon. A series of cuts is created in the tendon to allow it to stretch and lengthen.
Ankle Fracture Surgery
This surgery fixes an unstable break in your ankle. The break could be in the small bone of your lower leg, called the “fibula” or the larger bone, called the “tibia.” Sometimes, they’re both broken. Your surgeon will stabilize your bones so your ankle can heal.
Ankle Fusion, Transfibular
This surgical procedure is performed to treat severe arthritis or injury of the ankle joint. During the procedure, the surgeon removes damaged bone and cartilage and fuses the joint. This stabilizes the ankle and relieves pain.
Ankle Replacement
During this procedure, the surgeon removes diseased or damaged portions of the ankle. The surgeon implants an artificial ankle joint consisting of metal and plastic components. The new joint will help reduce pain and restore mobility to the ankle.
Arthroscopic Articular Cartilage Repair (Ankle)
This minimally-invasive procedure is performed to stimulate the growth of fibrocartilage in an injured joint. Fibrocartilage is a tough, dense, fibrous material that can fill in areas where smooth, glassy cartilage has become damaged or worn away. This procedure may be performed with general or regional anesthesia.
Arthroscopy of the Ankle
This procedure identifies and treats problems in your ankle. With it, the surgeon can access your ankle without creating a large incision.
Bunion Correction with Scarf and Akin Osteotomy
This procedure is used to correct a bunion, a deformity of the joint at the base of the big toe. During this procedure, portions of bone are removed and the bones of the foot and toe are aligned properly, eliminating the bump on the inner side of the foot.
Bunionectomy (Chevron Bunionectomy)
This outpatient procedure is performed to correct a bunion, a deformity of the toe joint. During the procedure, the surgeon may remove excess bone and then shift the toe into proper alignment. This surgery is commonly performed with regional anesthesia.
Bunionectomy With Wedge Osteotomy
This outpatient procedure is performed to correct a bunion, a deformity of the toe joint. This surgery is commonly performed with regional anesthesia.
Bunionette Deformity Correction (Distal Fifth Metatarsal Osteotomy)
This surgical procedure is performed to correct a bunionette, a bony bump on the outer side of the foot at the base of the fifth toe. During this procedure, the surgeon realigns the head of the metatarsal and removes excess bone to eliminate the prominence and give the foot a more natural shape.
Calcaneal Fracture Fixation (Open Reduction and Internal Fixation)
This procedure is used to correct a severe fracture of the calcaneus (the heel bone). During this procedure, the surgeon stabilizes the bone with hardware to allow the bone to heal properly.
Calcaneal Sliding Osteotomy (with Lateral Plate Fixation)
This procedure changes the alignment of the calcaneus, commonly called the “heel bone.” The surgeon will cut this bone, adjust its position and stabilize it with an implant. This technique can be used to correct problems such as a flat foot or an abnormally high arch.
Charcot Foot Treatment Options
Charcot foot is a deformity that can result as a complication of diabetes and other conditions. It develops after you lose sensation in your legs and feet. The joints and bones of your foot begin to break down and collapse. You cannot feel these injuries, and you may continue to walk on the foot. This worsens the damage. Charcot foot is a disabling deformity. It can be difficult to treat, but there are techniques that can be used to correct it.
Cheilectomy
This surgical procedure is used to help relieve symptoms of hallux rigidus by removing bony growths on top of the big toe’s main joint. This procedure improves joint movement and is most successful in patients with less severe arthritis.
Cotton Osteotomy (Medial Cuneiform Opening Wedge Osteotomy)
This surgical procedure helps to create an arch in the foot. It is commonly performed to help correct the condition of pes planus (commonly called flat foot or fallen arch). A Cotton osteotomy can change the shape of your foot, giving it a more normal appearance.
Debridement of the Achilles Tendon
This outpatient procedure is designed to repair a damaged Achilles tendon. During the procedure, injured and scarred tissue is removed. This can reduce or eliminate the pain of tendinitis.
DuVries Arthroplasty
This procedure is used to correct deformities such as hammertoe and claw toe. The surgeon shortens a bone in the toe to allow the toe to straighten and return to a more natural posture.
Electromyography (EMG)
This is a test of your muscles and nerves. It usually has two parts. One is a nerve conduction study. This measures how well electricity moves through your nerves. The second part is a needle electromyogram. It records the electrical signals your muscles make when you move them. The results can help your doctor find problems linked to certain disorders or conditions.
Excision of Mortons Neuromas
Morton’s neuroma is an enlarged nerve, compressed or pinched between the bones and the ligament that holds them together. This procedure eases the pain by releasing pressure from the nerve or removing the nerve.
First Metatarsal-phalangeal Joint (MTP) Arthrodesis
This surgical procedure is performed to help relieve pain in the front of the foot and correct deformities in the MTP joint of the big toe caused by injury, arthritis or genetic defect. The procedure fuses the bone at the base of the big toe to the first metatarsal bone of the foot.
Gastrocnemius Recession (Intramuscular Approach)
This outpatient procedure is used in the correction of conditions such as flatfoot, chronic Achilles tendonitis, or equinus (commonly called toe walking). Gastrocnemius recession lengthens the muscles and tendons at the back of the leg, allowing the heel to shift downward into a more natural position. In many cases, this technique is performed as an alternative to Percutaneous Tendo-Achilles Lengthening, which can permanently weaken the Achilles tendon.
Haglund’s Deformity Surgery (Resection Method)
This treatment removes a bony bump on the back of your heel. That bump is called a “Haglund’s deformity.” It can cause heel pain.
Hammertoe Correction (PIP Joint Arthroplasty)
This surgical procedure is used to correct a hammertoe, a deformity of the toe that causes the toe to become permanently frozen in a bent position. During this procedure, a small piece of bone is removed to shorten the toe and allow it to straighten.
Jones Fracture Fixation (Intramedullary Screw)
This procedure is used to correct a Jones fracture – a fracture of the fifth metatarsal bone of the foot. During this procedure, the surgeon inserts a screw into the metatarsal to stabilize the bone and allow it to heal properly.
Kidner Procedure
During this outpatient procedure, the physician removes a problematic accessory navicular bone. The accessory navicular is an abnormal, unnecessary bone found in a small percentage of people. It is located on the inner side of the foot.
Lapidus Procedure for Bunion Correction
This procedure is used to correct a bunion, a bony bump at the base of the great toe caused by excess bone growth and misalignment of the bones of the foot and toe. This procedure removes the bump and brings the toe back into proper alignment.
Lateral Ankle Ligament Reconstruction
This procedure is performed to correct chronic ankle instability that has not responded to treatment such as physical therapy. Ankle instability occurs when ligaments are stretched or torn. A simple repair, known as the Bröstrom-Gould technique, is ideal for athletes who need to retain full range of motion.
Lateral Column Lengthening (Evans Osteotomy) for Adult Acquired Flatfoot
This surgical procedure is used to modify the shape of the foot, creating an arch to correct the condition of pes planus (commonly called flat foot or fallen arch). It can dramatically change the shape of the foot, giving the foot a more normal appearance.
Lisfranc Injury Surgery
This surgery repairs an injury of the Lisfranc joint complex. That’s a cluster of small bones and ligaments in the midfoot. This surgery stabilizes broken or dislocated bones.
Medial Calcaneal Sliding Osteotomy
This surgical procedure is used to modify the shape of the foot, creating an arch to correct the condition of pes planus (commonly called flat foot or fallen arch).
Metatarsal Fracture Fixation (Open Reduction and Internal Fixation)
This procedure is used to correct a fracture of one or more of the long bones of the foot. During this procedure, the surgeon stabilizes the bones with hardware to allow the bones to heal properly.
Midfoot Fusion
This surgical procedure is performed to help relieve pain in the foot and correct deformities in the midfoot caused by injury, trauma, arthritis, or genetic defect. The procedure fuses any combination of the navicular, cuboid and cuneiform bones in the midfoot.
Nerve Conduction Study (NCS)
This noninvasive, outpatient exam is used to measure how quickly nerves conduct electrical signals through the body. NCS is a valuable technique for diagnosing nerve damage. If damage exists, NCS can help a physician find its source.
Popliteal Fossa Block
This outpatient procedure numbs the lower leg with an injection of local anesthesia. Typically, it is used for surgery on the lower leg, ankle and foot.
PRP Therapy (Overview)
Platelet rich plasma therapy can help injured joints and other problems. It uses parts of your own blood to reduce pain and speed up healing.
Subtalar Fusion
This surgical procedure is used to help relieve pain in the joint beneath the ankle joint and correct deformities in the hindfoot caused by injury, arthritis, or genetic defect. The procedure fuses the calcaneus (the heel bone) to the talus, the bone that connects the foot to the ankle.
Subtalar Implant for Adult Acquired Flatfoot
This procedure is designed to limit hyperpronation, an excessive range of motion of the subtalar joint typically caused by hereditary underdevelopment of the talus or the calcaneus. Hyperpronation can allow the foot to collapse inward and downward. During this procedure, a small device is implanted between the talus and calcaneus to correct this abnormal motion and stabilize the ankle. Several implant styles are available.
Surgery for Achilles Tendon Rupture
This surgical procedure is used to repair a ruptured Achilles tendon, the large tendon that travels down the back of the ankle. This procedure will help the tendon heal properly, restoring function to the foot and ankle.
Talar Fracture Fixation (Open Reduction and Internal Fixation)
This procedure is used to correct a fracture of the talus, one of the three main bones that form the ankle joint. During this procedure, the surgeon stabilizes the bone with hardware to allow the bone to heal properly.
Tarsal Tunnel Decompression
This surgical procedure relieves pressure on the tibial nerve. This nerve passes through a space called the tarsal tunnel, which is found just behind the bony bump on the inner side of the ankle. The nerve can become compressed in this tunnel.
Tendon Transfer (FHL to Achilles)
This procedure repositions the flexor hallucis longus tendon, (commonly called the “FHL” tendon) to reinforce a diseased Achilles tendon. The FHL tendon travels along the inner side of the ankle and foot. It is responsible for flexing the big toe. Repositioning it adds strength to the Achilles.
Tibiotalocalcaneal Fusion (with Intramedullary Rod)
This surgical procedure fuses your ankle joint with a rod commonly called a “nail.” It passes through the bones of your foot and lower leg. This type of fusion can be helpful if you have severe arthritis or other serious problems with your ankle. It may also be needed if you have had a total ankle replacement that has failed.
TightRope™ Fixation for Ankle Syndesmosis
This technique is used to stabilize an ankle after injury. It can be used to repair a high ankle sprain, which damages the soft tissue structures between the tibia and fibula and causes these bones to separate. It can also be used to stabilize a fracture of the fibula. The TightRope system anchors the ends of the tibia and fibula together with a braided polyethylene cord, rather than with a rigid surgical screw, to restore the original position of the bones and to allow for proper healing.
Total Ankle Joint Replacement (Salto® Talaris)
This surgical procedure is performed to remove portions of the ankle that are diseased or severely injured and to implant a device that will help manage pain and restore mobility to the ankle.
Total Ankle Joint Replacement (STAR™ Mobile-Bearing)
This surgical procedure is performed to remove portions of the ankle that are diseased or severely injured and to implant a device that will help manage pain and restore mobility to the ankle.
Total Ankle Joint Replacement (Wright INBONE® II)
This surgical procedure is performed to remove portions of the ankle that are diseased or severely injured and to implant a device that will help manage pain and restore mobility to the ankle.
Triple Arthrodesis
This surgical procedure is used to help relieve pain in the ankle joint and correct deformities in the hindfoot caused by injury, arthritis, or genetic defect. The procedure fuses the three main joints in the hindfoot that allow side-to-side movement – the calcaneo-cuboid, talonavicular, and subtalar joints.
Weil Osteotomy for Claw Toe
This procedure relieves the symptoms of claw toe, persistent metatarsalgia, metatarsal phalangeal (MTP) joint synovitis or MTP subluxation by shortening the end of the metatarsal at the base of the affected toe. This provides room for the toe to relax and return to its normal position.
Conditions
Accessory Navicular Problems
An accessory navicular is an extra bone on the inner side of your foot. It’s connected to the bone we call the “navicular,” which helps form the foot’s arch. Most people don’t have an accessory navicular, and you can have one and not know it. But in some people, this extra bone causes problems.
Achilles Tendon Injuries
The Achilles tendons are thick and powerful bands of fibrous tissue. They connect your calf muscles to your heel bones. The tendons help you walk, run and jump. And that means they are under a lot of stress, making injuries to the Achilles tendons common.
Adult Acquired Flatfoot
This is a collapse of your foot’s arch. It happens over time, usually in just one foot but sometimes in both. As your arch collapses, the bones of your foot may gradually shift out of alignment. This can cause pain and other problems.
Ankle Sprains
Ligaments are fibrous, elastic bands of tissue that connect and stabilize the bones. An ankle sprain is a common, painful injury that occurs when one or more of the ankle ligaments is stretched beyond the normal range of motion. Sprains can occur as a result of sudden twisting, turning or rolling movements.
Bunion
This deformity affects the joint at the base of the big toe. It is a bony bump beneath the skin on the inner side of the foot. A bunion starts small, but over time it can grow to become very large. Bunions are more common in women.
Bunionette Deformity (Tailor’s Bunion)
This bony bump forms on the outer side of the foot at the base of the fifth toe. Like a traditional bunion, a bunionette can be sore and painful. The skin covering the bump can become red and irritated.
Cavus Foot (High-Arched Foot)
This condition is an abnormally high arch of the foot that results in an excessive amount of body weight being directed to the ball and heel of the foot. Cavus foot can be congenital or acquired, may develop at any age, and can affect one or both feet.
Charcot-Marie-Tooth Disease (CMT)
This disease, one of the most common inherited neurological disorders, affects motor and sensory nerves throughout the body. It is usually not life-threatening, and rarely affects the brain. CMT is also called hereditary motor and sensory neuropathy (HMSN), or peroneal muscular atrophy.
Charcot’s Neuroarthropathy (CN)
This condition, which most often occurs as a complication of long-term diabetes, is a progressive degenerative condition that affects the foot. It is characterized by nerve damage in the foot along with severely weakened foot bones. This combination can result in a person fracturing the foot, but continuing to walk on the broken bones, which leads to debilitating foot deformity.
Claw Toe
This is a common foot deformity. With it, one or more toes buckle and curl into a claw shape. Over time, a claw toe can become locked in this position. It can dig into the sole of your foot. You may have trouble finding comfortable shoes.
Diabetic Foot
This term is used to describe foot problems that stem from diabetes. These problems can be difficult to treat.
Fracture of the Heel Bone (Calcaneus)
This condition is a break in the heel bone, called the calcaneus, which forms the back of the foot. This bone supports the foot and is important for normal walking.
Fracture of the Talus
This condition occurs when the talus, a bone that connects the foot and ankle, develops a fracture from a severe impact or fall. The talus is an important bone of the foot, as it aids in walking on uneven ground and in weight transfer across the ankle joint.
Gout
This is a form of arthritis. It causes pain and swelling in your joints. For many people, it starts in the big toe.
Haglund’s Deformity (Retrocalcaneal Bursitis)
This condition is a bony enlargement on the back of the heel that can aggravate the retrocalcaneal bursa, a fluid-filled sac located on the back of the heel between the Achilles tendon and the calcaneus. The bursa can become inflamed and swollen, a condition called bursitis. Haglund’s deformity most commonly affects young women.
Hallux Rigidus (Stiff Big Toe)
This is a type of arthritis that affects the base of the big toe. It forms in the metatarsophalangeal joint (we call it the “MTP” joint). With hallux rigidus, the protective cartilage on the ends of these bones wears away. Bone rubs against bone. Bony growths called “bone spurs” may form. Your toe stiffens, and this can make walking uncomfortable.
Hammer Toe
This condition is a deformity in which a toe bends downward at the middle joint. The second toe is the one most likely to be affected, but this deformity can occur in other toes as well. Sometimes, more than one toe is affected.
High Ankle Sprain (Syndesmosis Ligament Injury)
This condition is a sprain of one or more of the ligaments that hold the tibia and fibula together at the ankle. This joint, called the ankle syndesmosis, is made up of ligaments on the front and rear of the ankle, and in the space between the tibia and fibula.
Jones Fracture
This is a break of a bone in the foot called the “fifth metatarsal.” It’s on your foot’s outer side, behind the little toe. With a Jones fracture, this bone breaks on the end furthest from the toe. The fifth metatarsal doesn’t have a good blood supply there, so healing can be difficult.
Lisfranc Injury
This is an injury of the middle part of the foot, where the metatarsal bones of the forefoot connect to the cuneiform bones of the midfoot. It can involve torn ligaments, broken bones or a combination of both. And, it can involve more than one joint.
Metatarsalgia
The ball of your foot absorbs a lot of stress when you run and jump. It can become injured and sore. We call this pain “metatarsalgia.” The pain can keep you from exercising and from playing sports. And it can be a problem for active people.
Morton’s Neuroma
This condition is a thickening of the nerve sheath that surrounds a nerve in the ball of the foot. It most commonly develops between the third and fourth toes. It also commonly occurs between the second and third toes.
MTP Synovitis (Capsulitis)
This condition is a sharp or aching pain in the ball of the foot that is most often centered beneath the base of the second toe. This pain is an indication that the bone at the base of the toe, called the proximal phalanx, is beginning to separate from the long bone of the foot, called the metatarsal.
Muscle Strain of the Calf (Gastrocnemius / Soleus Strain)
This common injury is a stretching or tearing of the gastrocnemius or soleus muscles of the lower leg. One or both muscles may be affected.
Osteochondral Injuries of the Talus
The talus, lined with articular cartilage, connects to the tibia and fibula to make up the ankle joint. An osteochondral injury occurs when the talus and/or surrounding cartilage is bruised, fractured, or chipped from an injury.
Osteomyelitis
If you have an infection in a bone, you have osteomyelitis. It’s a serious condition that can cause part of your bone to die. And, the infection can spread to other parts of your body.
Peroneal Tendon Tears
This condition is a tearing of one or both peroneal tendons, which travel down the lower leg, behind the lateral malleolus and along the outer side of the ankle.
Pilon Fractures
This injury is a fracture at the base of the tibia (the largest of the two bones in the lower leg). Pilon fractures involve the weight-bearing surface of the tibia, and typically occur just above the ankle. In many cases, when the tibia is fractured, the thinner bone in the lower leg (called the fibula) is also broken.
Plantar Fasciitis
Plantar fasciitis is an irritation of the plantar fascia. This thick band of connective tissue travels across the bottom of the foot between the toes and the heel. It supports the foot’s natural arch. It stretches and becomes taut whenever the foot bears weight.
Posterior Tibial Tendon Dysfunction (PTTD)
This condition is an overstretching and inflammation of the posterior tibial tendon, which travels from a muscle in the calf down to the arch of the foot. This tendon is one of the major supporting structures of the foot’s arch and aids in walking.
Rheumatoid Arthritis (RA) of the Foot and Ankle (Arthritis Foundation Approved)
Rheumatoid arthritis, a condition that can attack joints throughout the body, commonly affects both feet and both ankles at the same time. It can cause the joints to become swollen and possibly deformed, causing disability.
Sesamoiditis
This injury involves two small bones under the foot near the big toe. They are called “sesamoid” bones. They aren’t directly connected to other bones of the foot. Instead, the sesamoids are embedded in tendons. With sesamoiditis, these bones and the tendons around them become irritated and inflamed.
Stress Fractures of the Foot and Ankle
Stress fractures are one or more tiny cracks in a bone. These fractures are common in the legs and feet. That’s because your legs and feet have to support your weight and absorb the forces of walking, running and jumping.
Tarsal Tunnel Syndrome (Posterior Tibial Neuralgia)
This condition, also called TTS, affects the tibial nerve in the ankle. This nerve is a branch of the sciatic nerve. It passes from the leg down to the foot. Just below the bony bump on the inner side of the ankle, it passes through a small space called the tarsal tunnel. TTS is a compression of the nerve within this tunnel.
Hand
Care and Management
Basal Joint Surgery
Pain in the basal joint caused by arthritis makes it difficult for patients to grip and hold or twist objects between the thumb and fingers. This surgical procedure removes and rebuilds the basal joint.
Carpal Tunnel Release (Open Technique)
This surgical procedure treats the pain of carpal tunnel syndrome. It relieves pressure on a nerve that travels through your wrist. This nerve is called the “median” nerve.
De Quervain’s Release
This outpatient procedure relieves the symptoms of De Quervain’s tenosynovitis by releasing the tendon sheath that wraps around the tendons at the base of the thumb. This relieves pressure and friction on the tendons, allowing them to glide freely.
Digital Nerve Repair
This microsurgical procedure is used to reconnect the severed ends of a nerve in the hand to allow the nerve to heal and to reduce the possibility that a neuroma will form. Nerve repair can help restore sensation and muscle function, however, in many cases normal sensation and function is not fully restored.
Distal Radius Fracture Repair with Volar Plate
This procedure uses a metal implant to stabilize a fracture in the radius near the wrist. The radius is the largest of the two bones of the forearm.
Endoscopic Carpal Tunnel Release
This procedure is performed to relieve pressure on the median nerve, alleviating the pain of carpal tunnel syndrome and restoring normal sensation to the hand and fingers. The endoscopic technique, performed on an outpatient basis, creates less pain and scarring than traditional open surgery and allows for a quicker recovery.
Ganglion Cyst Removal
This outpatient procedure is used to remove a ganglion cyst, a fluid-filled sac that forms as a herniation from a joint capsule, ligament or tendon sheath. Ganglion cysts commonly develop at the wrist.
Needle Aponeurotomy for Dupuytren’s Contracture
This minimally-invasive, non-surgical office procedure is used to help straighten fingers that have become bent by Dupuytren’s contracture. A small needle is used to cut the contracted cords that cause the contracture and prevent the finger from fully extending.
Scaphoid Fracture Open Reduction and Internal Fixation (ORIF)
This procedure stabilizes a fractured scaphoid bone with screw fixation. The scaphoid is an important carpal bone of the wrist, which is critical in coordinating motion of the other carpal bones and the radius.
Tendon Repair
This procedure, performed under general anesthesia, is used to repair a ruptured or severed tendon in the finger or thumb.
Trigger Digit Release
During this minimally-invasive procedure, the surgeon opens a narrowed tendon pulley at the base of a finger or thumb affected by trigger digit. Opening the pulley prevents the nodule from catching, allowing the the affected digit to flex and extend normally with no triggering or pain.
Wrist Arthroscopy
This minimally invasive outpatient procedure allows the surgeon to evaluate and treat injuries and disorders of the ligaments, cartilage, and bones of the wrist. The surgeon uses a small camera, called an arthroscope, and tiny instruments which are inserted through small incisions in the wrist.
Conditions
Basal Joint Osteoarthritis
This condition is a degeneration of cartilage in the joints at the base of the thumb, collectively called the basal joint. The main component of the basal joint is the thumb carpometacarpal (CMC), joint. This joint, which allows the thumb to pivot and swivel, can wear out even early in life.
Carpal Tunnel Syndrome
Pain, numbness and tingling in your hand may be from carpal tunnel syndrome. It happens when the area around the main nerve to your hand is too tight. The nerve is called the median nerve. And the small space in your wrist where it passes is called the carpal tunnel.
De Quervain’s Tenosynovitis
This condition, also called stenosing tenosynovitis of the first dorsal compartment of the wrist, is an inflammation of the sheath that wraps around the tendons at the thumb side of the wrist.
Digital Mucous Cysts
A mucous cyst is a small, fluid-filled sac that forms on the back of the finger near the base of the fingernail. It is a form of ganglion cyst that erupts from the capsule of the joint at the end of the finger, called the DIP joint. The cyst is attached to the joint capsule by a “stalk” that allows fluid to move into the cyst from the joint. Mucous cysts most commonly affect the index finger of the dominant hand.
Distal Radius Fracture (Broken Wrist)
This condition is a break of the radius bone at the wrist. The radius is the larger of the two bones that connect the wrist to the elbow. The other bone is called the ulna. The radius supports the majority of forces at the wrist joint with its large joint surface. A fracture of the distal end of the radius – the end nearest the wrist -is one of the most common types of fractures. It may be part of a complex injury that involves other tissues, nerves and bones of the wrist.
Dupuytren’s Disease
This condition is a thickening of the fascia on the palm of the hand. The fascia is a connective tissue located just beneath the skin of the palm and fingers. This thickened fascia can form lumps or nodules under the skin, or long thick cords of tissue that extend from the palm to the fingers. Often, this thickened tissue contracts. This causes one or more fingers to curl toward the palm. This is called a flexion contracture.
Finger Dislocation
If your finger is dislocated, that means a bone has been forced out of its normal position. It’s a common, painful injury, and one that needs proper treatment.
Finger Fracture
If you’ve fractured a finger, you’ve broken one or more of the finger bones we call “phalanges.” Each individual bone is called a “phalanx.” You’ve got three in each finger, and two in each thumb. They are supported by a network of soft tissues that can also be damaged during a fracture.
Fingertip Injuries
Our fingers are often in harm’s way, and our fingertips are prone to injury. A fingertip injury can involve skin, soft tissue, nerves and bone. It can involve the nail and the nailbed. These injuries can be serious, painful, and slow to heal. If you’ve injured your fingertip, you can take a few simple steps to minimize problems.
Flexor Tendon Injuries
The flexor tendons of the hand are responsible for flexion of the fingers and thumb toward the palm. These long structures are connected to the flexor muscles in the forearm. An injury to one of these tendons can cause pain and inability to flex the finger or thumb and grasp with the hand. Common flexor tendon injuries include lacerations, ruptures and inflammation.
Fractures of the Hand (Metacarpal Fractures)
This condition is a fracture, or break, of one or more of the metacarpal bones of the hand. The fracture may be nondisplaced, in which the bones remain aligned, or displaced, in which the fractured ends shift out of alignment. Without proper treatment, the bones may not heal correctly. This can result in improper alignment of the fingers, leading to poor hand function.
Ganglion Cysts of the Hand
A ganglion cyst is a fluid-filled sac that forms as a herniation from a joint capsule or tendon sheath. The sac is attached to the joint or tendon sheath by a “stalk” that allows fluid to move into the pouch from the joint or sheath. The stalk functions as a valve and often limits fluid drainage out of the cyst, allowing the cyst to increase – but not decrease – in size. In some cases the stalk functions as a two-way valve, allowing fluid to travel in both directions. This can enable the cyst to increase and decrease in size based on activities.
Mallet Finger
This condition is an injury to the end of the extensor tendon that straightens the finger’s end joint, called the DIP joint. It results in drooping of the fingertip, and prevents the finger from being straightened.
Nerve Injuries of the Hand
Complex networks of nerves travel through your hands and fingers. If you injure a hand or a finger, you can damage these delicate nerves. Without proper care, a nerve injury can cause permanent problems.
Rheumatoid Arthritis (RA) of the Hand (Arthritis Foundation Approved)
Rheumatoid arthritis, a condition that can attack joints throughout the body, commonly affects the joints and surrounding tendons of the wrist and fingers. It can cause the joints to become swollen, painful and possibly deformed, interfering with normal hand function and significantly impacting a person’s quality of life.
Scaphoid Fractures
A scaphoid fracture, one of the most common types of wrist fractures, is a break in the scaphoid bone. The scaphoid, one of the most important bones in the wrist, has a limited blood supply. An improperly treated scaphoid fracture can result in significant wrist pain, arthritis, and loss of motion.
Thumb Ulnar Collateral Ligament (UCL) Injury
This condition, also called skier’s thumb, is an acute sprain or tear of the ulnar collateral ligament (UCL) on the ulnar side of the metacarpal-phalangeal (MCP) joint of the thumb. A related condition, called gamekeeper’s thumb, is a chronic injury that develops over time from repeated stretching of the UCL.
Triangular Fibrocartilage Complex (TFCC) Tears
This condition is a degenerative or traumatic tear of one or more parts of the triangular fibrocartilage complex (TFCC), which stabilizes the ulna. The TFCC is composed of a group of ligaments that form connections between the radius, ulna and the carpal bones of the hand. At the center of these ligaments lies the most commonly injured structure, the triangular fibrocartilage disc, which is connected between the radius and the base of the ulnar styloid.
Trigger Digit
This common condition, also known as stenosing tenosynovitis, is a narrowing of a portion of the tendon sheath in the finger or thumb that interferes with normal finger movement. This condition most commonly affects the ring finger, but can affect any digit. It is more common in middle-aged women, but anyone can be affected, even newborns.
Hip and Thigh
Care and Management
Femoroacetabular Impingement Surgery (Arthroscopic Method)
This surgery fixes problems caused by a poorly-shaped hip joint. That’s a condition known as femoroacetabular impingement. We call it “FAI.” The surgeon will repair your hip without making a large incision.
Hip Arthroscopy
This outpatient procedure is an examination of the inside of the hip joint. The surgeon uses miniature instruments and a small camera (called an arthroscope) to see inside the joint. Arthroscopy can be used to diagnose and treat problems of the joint.
Hip Fracture Treatment with Surgical Screws
This surgical procedure uses metal surgical screws to repair a fracture of the femur. This procedure is typically used for patients who have minimal damage to the bone and minimal shifting from the fracture.
Hip Hemiarthroplasty (Bipolar)
This surgical procedure replaces the head of a damaged femur with an implant designed to stabilize the femur and restore hip function. Unlike total hip replacement, in which both the ball of the femur and the hip socket are replaced, in this procedure, only the ball is replaced.
Hip Joint Injection
If you have pain in your hip, your doctor may inject medicine into your hip joint. It can help your doctor find where your pain is coming from. It can also make your hip feel better.
Living With Osteoarthritis of the Hip
When you have osteoarthritis of the hip, sometimes it’s hard to be as active as you like. But you can still do many of the things you enjoy. You just have to know how to manage your condition.
Mini Total Hip Replacement
This procedure uses a small incision to replace the diseased and damaged portion of the hip joint. Patients feel less pain and recover more quickly compared to patients who undergo traditional hip replacement surgery, which requires a longer incision. While this procedure uses specialized surgical tools, the implants used are the same as the ones used in traditional surgery.
Partial Hip Resurfacing (Wright)
This surgery replaces the diseased and damaged parts of the femur (thigh bone) with a metal ball component.
PRP Therapy (Overview)
Platelet rich plasma therapy can help injured joints and other problems. It uses parts of your own blood to reduce pain and speed up healing.
Revision Hip Surgery
This surgery replaces worn artificial hip parts and damaged bone with new metal, plastic or ceramic components. The new components restore normal hip joint stability.
Total Hip Replacement
During this procedure, your damaged hip joint is replaced with implants that recreate the ball and socket of a healthy hip. This can reduce pain and restore your hip function.
Total Hip Replacement, Anterior Approach
This surgery replaces diseased and damaged portions of the hip with implants designed to restore function to the hip joint. The surgeon uses an incision on the anterolateral part of the hip, instead of a more traditional incision on the side or back of the joint.
Conditions
Anatomy of the Hip Joint
The hip joint is one of the largest weight-bearing joints in the body. This ball-and-socket joint allows the leg to move and rotate while keeping the body stable and balanced. Let’s take a closer look at the main parts of the hip joint’s anatomy.
Avascular Necrosis (Osteonecrosis) of the Hip
This is a weakening and collapse of the bone in the head of your femur. That’s the ball that fits in the socket of your hip. As this bone gradually dies and breaks apart, you can develop painful arthritis in your hip.
Bursitis of the Hip (Trochanteric Bursitis)
This is an irritation or swelling of the trochanteric bursa. This small, fluid-filled sac is found on the outer side of the femur. It acts as a cushion for the iliotibial band, a thick tendon in your leg.
Femoroacetabular Impingement (FAI)
This is a problem with the hip joint. In a healthy hip, the ball of the femur is smooth and round. It fits perfectly into the hip socket. But with this condition, the ball, the socket or both the ball and the socket are shaped poorly. They don’t fit together well. When you move your hip, they rub together harmfully.
Femur Fractures
The thigh bone, also called the “femur”, is the largest and strongest bone in your body. A femur fracture is a crack or a break of this bone.
Hamstring Muscle Injuries
The hamstrings are three powerful muscles that travel along the back of your thigh. They are the semitendinosus, the semimembranosus and the biceps femoris muscles. They help bend your knee and extend your leg behind your body. Because these muscles handle high loads of stress, they are susceptible to stretching and tearing. This is called a muscle “strain.” Hamstring strains are common among runners, dancers, and athletes who play sports that require sudden starts and stops.
Hip Fracture
This is a break of the upper part of your femur. The femur is the long bone in your upper leg. At the top of the femur is the “head.” This is the ball that fits into your hip socket. A hip fracture may happen at the “neck” of the femur (the thin portion of bone under the head). Fractures may also happen below the neck.
Hip Fracture Prevention
A broken hip is serious and disabling. With a broken hip, you may not be able to care for yourself. Sometimes, complications from a hip fracture can lead to death. Avoid a broken hip with these basic safety measures.
Iliotibial Band Syndrome (ITBS)
This is a problem on the outer side of your thigh. It’s an inflammation of the iliotibial band. That’s a thick band of tissue that spans from your hip to your shinbone. When this band becomes in inflamed, it can hurt.
Inflammatory Arthritis of the Hip
This is a type of arthritis that can affect people of all ages. It’s not the same as the most common form of arthritis, called “osteoarthritis.” That type commonly comes from wear and tear. Inflammatory arthritis can develop without any wear and tear at all.
Labral Tear of the Hip (Acetabular Labrum Tear)
If your hip joint hurts, or if it catches or clicks when you move your leg, you may have a torn labrum. That’s a rim of tissue that surrounds the hip’s socket. It helps to deepen the socket and cushion the joint. A torn labrum can keep the hip joint from working smoothly.
Loose Bodies in the Hip
Loose bodies are pieces of cartilage or bone of various sizes that have broken away and become trapped in a joint. Loose bodies usually have an irregular shape, but over time they may be worn down into a smooth, spherical or disc-shaped mass.
Muscle Strain Injuries of the Hip
The hip is where the femur meets the pelvis. Several strong muscles are found here. They handle high loads of stress. They may suffer from overstretching and tearing. This is called a muscle “strain.” It’s a common injury among athletes who play sports that require sudden starts and stops.
Muscle Strain Injuries of the Thigh
Your thigh has groups of powerful muscles. The quadriceps, the adductors and the hamstring muscles handle high loads of stress. They may suffer from overstretching and tearing. This is called a muscle “strain.” It is a common injury among athletes who play sports that require sudden starts and stops.
Snapping Hip
This is a snapping or a popping sensation in your hip. It may happen when you stand up, when you walk, or when you move your leg a certain way.
Sports Hernia
This is a strain or a tear of soft tissue. It often involves the muscles and tendons that travel from your lower abdomen to your pubic bone. A sports hernia does not create a hole in your abdominal wall. This injury can be difficult to diagnose, because it does not cause a bulge in your skin.
Knee
Care and Management
ACL Reconstruction (Patellar Tendon Graft Technique)
This procedure repairs your knee after a tear of the anterior cruciate ligament (commonly called the “ACL”). This ligament is in the center of the knee. It helps anchor the femur to the tibia. This surgery can allow you to regain normal knee function.
Arthroscopy (Overview)
If you have a joint problem, your surgeon may want to try arthroscopy. This lets your surgeon see inside your joint with a small, thin camera called an “arthroscope.” It can be used on any joint, but let’s see it in the knee.
Cartilage Repair
This technique is designed to treat and repair cartilage defects by regenerating the patient’s own hyaline cartilage, (a weight-bearing cartilage that lines the surface of the knee joint).
Loose Body Removal (Knee)
During this minimally-invasive outpatient procedure, the surgeon removes debris from within the knee joint. This debris is usually a piece of bone, cartilage or other tissue that has broken free and is floating within the joint.
Meniscal Transplant
This outpatient procedure is performed to replace lost or severely damaged meniscal cartilage in the knee joint. In a healthy knee, this cartilage is present in two c-shaped wedges called menisci. Each one is called a meniscus. These wedges help cushion and stabilize the knee. This procedure is performed under general anesthesia with the aid of a small camera, called an arthroscope, and miniature instruments.
Meniscus Repair (Arthroscopic Technique)
Each of your knee joints is cushioned by two c-shaped wedges of cartilage. The two cushions in each knee are called the “menisci.” Individually, each cushion is called a “meniscus.” Certain motions, such as twisting the knee, can cause a meniscus to tear. In many cases, a torn meniscus can be treated with arthroscopic surgery.
Microfracture Drilling Procedure for Isolated Chondral Defect
This minimally-invasive procedure repairs damaged cartilage in the knee joint. Small holes are drilled into the bone at the base of the damaged area to stimulate the growth of healthy “scar” cartilage.
Mini Incision Total Knee Replacement
Mini-incision Total Knee Arthroplasty, also called MIS TKA, replaces the damaged and painful areas of the knee joint with metal and polyethylene plastic parts. The MIS total knee procedure is performed through an incision that is smaller than the incision used for traditional total knee replacement surgery. This technique reduces blood loss and pain and allows for a shorter recovery.
Partial Knee Replacement (using OXFORD® implant)
Unlike total knee replacement surgery, this less invasive procedure replaces only the damaged or arthritic parts of the knee. The OXFORD® unicompartmental knee uses metal and plastic implants designed to potentially last longer and wear down less easily than traditional implants.
Partial Meniscectomy
The meniscus is a cushion of cartilage. There are two in each knee. If one of these shock absorbers is worn out or hurt, you may need a partial meniscectomy to remove the damaged areas.
Patellofemoral Replacement
This surgical procedure removes portions of damaged cartilage on the femur in the knee joint that have been rubbing against the underside of the patella, causing pain and loss of mobility. This cartilage is then replaced with a specially-designed implant.
Posterior Cruciate Ligament (PCL) Reconstruction
This surgical procedure replaces a damaged posterior cruciate ligament (PCL). The PCL is a band of tissue that connects the femur to the tibia inside the knee.
PRP Therapy (Overview)
Platelet rich plasma therapy can help injured joints and other problems. It uses parts of your own blood to reduce pain and speed up healing.
Revision Knee Surgery
This procedure replaces worn artificial knee parts and damaged bone with new metal and plastic components.
Total Knee Replacement
This procedure restores function to a severely damaged knee. Most commonly, it is used to repair a knee that has been damaged by arthritis. During the procedure, the surgeon replaces the damaged portions of the knee with artificial parts. These parts consist of a metal femoral component, a metal tibial component and a plastic spacer. A small plastic patellar component may also be used.
Conditions
Anatomy of the Knee
The knee is the body’s largest joint. It’s the place where three bones meet: the tibia, the femur and the patella. The knee is a “hinge” joint. It allows the leg to bend in one direction only. Let’s take a closer look at the main parts of the knee’s anatomy.
Anterior Cruciate Ligament (ACL) Injuries in Women
The anterior cruciate ligament, commonly called the ACL, is a thick, elastic band of tissue that runs from the bottom of the femur to the top of the tibia. It helps stabilize the knee joint. The ACL can become stretched or torn when the knee is twisted or hyperextended. For reasons that are not fully understood, ACL injuries are much more common in women than in men.
Anterior Cruciate Ligament Tear (ACL Tear)
This injury is a tearing of the ACL ligament in the knee joint. The ACL ligament is one of the bands of tissue that connects the femur to the tibia. An ACL tear can be painful. It can cause the knee to become unstable.
Bursitis of the Knee (Pes Anserine Bursitis)
This is a swelling of a fluid-filled sac called a “bursa.” It’s on the inner side of your knee, between the tibia and the tendons that attach to your hamstring muscle. You have similar sacs near other large joints throughout your body. They act as cushions between your bones and your soft tissues. Normally they have a small amount of fluid inside them. But sometimes they can swell. We call that “bursitis.”
Deep Vein Thrombosis (DVT)
This condition is a blood clot that forms in a vein deep inside the body. This type of clot most commonly develops in the legs. This condition is dangerous, because the clot can break free and travel through the bloodstream to the lungs.
Iliotibial Band Syndrome (ITBS)
This is a problem on the outer side of your thigh. It’s an inflammation of the iliotibial band. That’s a thick band of tissue that spans from your hip to your shinbone. When this band becomes in inflamed, it can hurt.
Lateral Collateral Ligament (LCL) Injury
This is a stretching or tearing of a ligament on the outer side of your knee. The lateral collateral ligament, commonly called the “LCL”, connects the femur to the fibula. The LCL helps stabilize your knee. This ligament, along with the medial collateral ligament, helps prevent excessive side-to-side movement of your knee joint. It helps keep the upper and lower leg aligned properly.
Medial Collateral Ligament (MCL) Injury
This is a stretching or tearing of a ligament on the inner side of your knee. The medial collateral ligament, commonly called the “MCL”, is connected to the femur and to the tibia. The MCL helps stabilize your knee. This ligament, along with the lateral collateral ligament, helps prevent excessive side-to-side movement of your knee joint. It helps keep the upper and lower leg aligned properly.
Meniscus Tear
This is a common injury of the knee. Your knee joint is cushioned by two c-shaped wedges of cartilage called the “menisci.” Each individual cushion is called a “meniscus.” This injury is a tear of one of these cushions.
Osgood-Schlatter Disease
This is a type of injury that causes knee pain in children. It’s an inflammation of a growth plate in the tibia. Growth plates are places where new bone tissue forms. They are found in the long bones of growing children. But growth plates are weaker than the surrounding bone. That makes them easier to injure.
Osteoarthritis of the Knee
Osteoarthritis, also called degenerative arthritis, is a gradual breakdown of cartilage in the joints. Cartilage is a tough, flexible connective tissue that protects the ends of bones in the joints. Osteoarthritis is common in the knees because the knees bear the weight of the body. Osteoarthritis of the knee can severely impact a person’s lifestyle.
Patellar Fracture
This is a break of the patella. That’s the small bone in the front of your knee often called the “kneecap.” The kneecap protects the joint and helps link your thigh muscles to your lower leg. A fracture can cause pain and other problems.
Patellar Tendinitis
This is a pain you feel just below your patella (the bone we commonly call the “kneecap”). It’s an injury to your patellar tendon, which connects the bottom of the kneecap to the shinbone.
Patellar Tendon Tear
This is a tear of a large tendon in the front of your knee. We call it the “patellar tendon.” It connects the bottom of the kneecap to the top of the shinbone. It helps you straighten your leg. You can have a tear that doesn’t go all the way through the tendon, or you can tear the tendon completely. A complete tear is a disabling injury.
Patellofemoral Pain Syndrome
This is a pain you feel in the front of your knee. It involves the patella. That’s the bone we commonly call the “kneecap.” The patella slides up and down in a groove on your femur as you bend and extend your knee. If you have this syndrome, you may have injured the soft tissues that support and cushion your kneecap. Or, you may have some damage to the cartilage on the underside of the kneecap.
Posterior Cruciate Ligament (PCL) Injuries
Strong bands of tissue called “ligaments” help stabilize the bones that form the knee joint. One of these ligaments is called the “PCL.” It helps connect the femur to the tibia. If you stretch or tear a PCl, your knee may become unstable.
Shoulder
Care and Management
Acromioclavicular (AC) Joint Separation Repair
This surgery repairs a severe separation injury of the AC joint in your shoulder. This is where your clavicle meets your scapula. With a severe separation injury, the ligaments that connect these bones are torn. The clavicle shifts out of position.
Bankart Repair
If you have a painful shoulder, you may have a torn labrum. That’s a tear of the thick band of tissue around your shoulder socket. A torn labrum can be fixed with a procedure called a “Bankart repair.”
Biceps Tenodesis
This surgery repairs a biceps tendon in your shoulder. It fixes a tendon that is partially torn, or completely torn, from the bone.
Distal Clavicle Excision (Resection, Arthroscopic Technique)
During this minimally-invasive procedure, the surgeon removes the end of the clavicle at the acromioclavicular joint in the shoulder. Removing this portion of bone will decompress the joint. It will help relieve the pain and loss of motion caused by arthritis or impingement. This procedure is performed with a small camera, called an arthroscope, and miniature instruments.
Glenohumeral Debridement
This minimally-invasive procedure is used to remove tissue in the shoulder joint that has been damaged from arthritis, overuse or injury. The physician uses a small camera, called an arthroscope, which is inserted into the shoulder joint.
Mini-Open Rotator Cuff Repair
This surgical procedure is used to inspect and reattach torn tendons in the shoulder’s rotator cuff. The initial part of the surgery is performed arthroscopically through small tubes. An open incision may be needed if the damage is severe.
PRP Therapy (Overview)
Platelet rich plasma therapy can help injured joints and other problems. It uses parts of your own blood to reduce pain and speed up healing.
Reverse Total Shoulder Replacement
During this procedure, the surgeon replaces a damaged shoulder joint with artificial components that reverse the structure of the shoulder. This procedure is most often used for patients who have had a failed total shoulder replacement. It is also helpful for patients who have had a complete tear of the rotator cuff, especially those whose injuries have led to an arthritic condition called cuff tear arthropathy.
Rotator Cuff Repair (Arthroscopic)
This surgery repairs a tear of the rotator cuff in your shoulder. The rotator cuff is group of muscles and tendons. It holds the head of the humerus in the shoulder socket.
SLAP Repair
This arthroscopic procedure is performed to repair a tear of the biceps tendon at the point where it connects to the labrum, a ring of cartilage that surrounds the shoulder socket. A tear at this point is called a SLAP (Superior Labrum Anterior-Posterior) tear. SLAP repair is performed under general and regional anesthesia, and patients usually leave the hospital the same day.
Subacromial Decompression
This surgery treats subacromial impingement. That’s a pain you feel when you raise your arm. It happens when tendons in your shoulder press and rub against a part of your shoulder blade called the “acromion.” This surgery is commonly done with the help of a special camera called an “arthroscope.”
Conditions
Acromioclavicular (AC) Joint Arthritis
This arthritis affects a joint at the top of your shoulder. It’s where the shoulder blade’s bony protrusion (called the “acromion”) meets the clavicle. This joint acts as a pivot point when you raise your arm above your head.
Biceps Tendon Tear (at the Shoulder)
Tendons are strong bands of tissue that connect muscle to bone. With this injury, one of the tendons anchoring your biceps muscle is torn. It may be torn partially or completely. Because the biceps is attached with two separate tendons, you may find that you can still use your biceps muscle even if one tendon is completely torn.
Biceps Tendonitis
This is a problem with a tendon in your shoulder. Most often, it’s the “long head of biceps” tendon. It travels from the front of your upper arm to the top of your shoulder socket. With this condition, the tendon becomes painfully inflamed or irritated.
Burners and Stingers
These are warm or painful sensations caused by an injury to the brachial plexus. This is a network of nerves that passes through your shoulder. They travel down your arm and to your hand.
Bursitis of the Shoulder (Subacromial Bursitis)
This is a swelling of a fluid-filled sac called the “subacromial bursa.” It’s in the shoulder, between a bony protrusion called the “acromion” and the rotator cuff. You have similar sacs near other large joints throughout your body. They act as cushions between your bones and your soft tissue. Normally they have a small amount of fluid inside them. But sometimes they can swell. We call that “bursitis.”
Clavicle Fracture (Broken Collarbone)
This is a common shoulder injury. It’s a break of the bone that rests between the shoulder blade and the sternum. We call it the “collarbone.” Your collarbones help connect your arms to your body.
Frozen Shoulder (Adhesive Capsulitis)
This is stiffening of your shoulder. It happens over time, and you may not know what caused it. With a frozen shoulder, it can be hard for you to be as active as you like.
Proximal Humerus Fracture (Broken Shoulder)
This condition is a fracture of the head of the humerus – the “ball” of the shoulder’s ball-and-socket.
Rotator Cuff Injuries
The rotator cuff muscles and tendons hold your upper arm bone in your shoulder socket. A hard fall, repetitive arm motions or problems with the structure of your shoulder can injure the rotator cuff.
Rotator Cuff Tear
The rotator cuff is a group of muscles and tendons in each shoulder. It holds your upper arm bone in your shoulder socket. It keeps your arm stable while allowing it to lift and rotate. Too much stress on the rotator cuff can cause a tear. This can be a painful injury.
Shoulder Dislocation
The shoulder is a ball-and-socket joint. The ball of your upper arm bone fits into a socket in your shoulder blade. If the ball slips out, your shoulder has “dislocated.”
Shoulder Impingement Syndrome
This is a painful pinching of soft tissues in your shoulder. It happens when these tissues rub and press against a part of your shoulder blade called the “acromion.” This can irritate your rotator cuff tendons, and also a soft sac called the “subacromial bursa.”
Shoulder Separation
This is an injury of the acromioclavicular joint (commonly called the “AC” joint). This is the joint where the clavicle meets the scapula. A shoulder separation is a stretching or a tearing of the ligaments that support these bones. This allows the bones to move out of position.
SLAP Tear (Superior Labrum from Anterior to Posterior Tear)
This is a shoulder injury. It’s a tear of the labrum. That’s a ring of cartilage that surrounds the shoulder socket and helps hold the head of the humerus in place. This type of tear happens where the biceps tendon attaches to the labrum.
Spine
Conditions
Cervical Radiculopathy
This condition is an irritation or compression of one or more nerve roots in the cervical spine. Because these nerves travel to the shoulders, arms and hands, an injury in the cervical spine can cause symptoms in these areas. Cervical radiculopathy may result from a variety of problems with the bones and tissues of the cervical spinal column.
Compression Fractures of the Spine
This is a collapse of vertebral bone. It can affect one or more vertebrae. Compression fractures typically develop in your mid or lower back. This can change the shape of your spine.
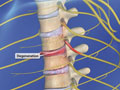
Herniated Discs
A herniated disc is a common injury that can affect any part of the spine. A herniated disc can cause severe pain and other problems in the arms or legs.
Kyphosis
This condition is a deformity of the spine. With it, your vertebrae change from a cylindrical shape to a wedge shape. Your spine may begin to curve forward. Eventually, this gives your upper back a rounded appearance.
Lumbar Radiculopathy (Sciatica)
This condition is an irritation or compression of one or more nerve roots in the lumbar spine. Because these nerves travel to the hips, buttocks, legs and feet, an injury in the lumbar spine can cause symptoms in these areas. Sciatica may result from a variety of problems with the bones and tissues of the lumbar spinal column.
Scoliosis
This condition is an abnormal curvature of the spine. It most often develops in early childhood, just before a child reaches puberty.
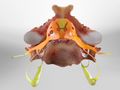
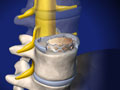
Spinal Stenosis
The spinal column contains open spaces that create passageways for the spinal cord and the spinal nerves. Spinal stenosis is a narrowing of (or an intrusion into) these openings. This can cause a compression of the nerves. Spinal stenosis most commonly affects the cervical and lumbar regions of the spine.
Spinal Stenosis (Cervical)
This condition is a narrowing of the spinal canal that results from the degeneration of bones, discs, or joints in the cervical spine.
Spinal Stenosis (Thoracic)
This condition affects the thoracic spine between the neck and the lower back. It is a narrowing of the spinal canal that results from degeneration of bones in the spine, disc herniation, or thickening of the tissues that surround the spinal cord.
Spondylolisthesis
This condition occurs when a lumbar vertebra slips out of place. It slides forward, distorting the shape of your spine. This may compress the nerves in the spinal canal. The nerves that exit the foramen (open spaces on the sides of your vertebrae) may also be compressed. These compressed nerves can cause pain and other problems.
Spondylosis
This condition is a degeneration of the spine that can affect the spine at any level, resulting in pain and discomfort that can grow worse over time.
Where Lower Back Pain Begins
Lower back pain is a common problem that severely impacts the quality of your life. It can limit your ability to be active. It can cause you to miss work. Many different causes may lead to pain in your lower back.
Where Neck Pain Begins
Neck pain is a common problem that severely impacts the quality of your life. It can limit your ability to be active. It can cause you to miss work. Many different causes may lead to pain in your neck.
Non-Surgical Care and Management
Surgical Care and Management
ALIF: Anterior Lumbar Interbody Fusion
ALIF is generally used to treat back or leg pain caused by degenerative disc disease. The surgeon will stabilize the spine by fusing vertebrae together with bone graft material.
Anterior Cervical Discectomy and Fusion (ACDF)
This surgery removes a herniated or degenerative vertebral disc in your neck and replaces it with a bone graft. This can relieve painful pressure on spinal nerves.
Artificial Cervical Disc Replacement
This procedure replaces a degenerative or damaged spinal disc with an implant designed to preserve motion in your neck. This procedure can relieve the pain of compressed nerves in the cervical spine.
Cervical Posterior Foraminotomy
This surgery creates more space for a compressed spinal nerve in your neck. The procedure relieves painful pressure caused by a herniated or degenerative disc.
Kyphoplasty (Balloon Vertebroplasty)
This minimally-invasive procedure repairs a vertebral compression fracture. It helps restore the spine’s natural shape. Some patients experience rapid pain relief after the procedure.
Laminectomy
This procedure relieves pressure on the nerve roots in the spine. It is most commonly performed to relieve the pain of stenosis. This is a narrowing of the spinal canal that is often caused by the formation of bony growths that can press against the nerve roots. The surgeon may treat one or more vertebrae.
Lumbar Discoscopic Discectomy
This minimally-invasive procedure is designed to relieve pain caused by herniated discs pressing on nerve roots. This surgery is performed through a small tubular device under local or epidural anesthesia, allowing the patient to leave the hospital the same day.
Spinal Fusion (Lumbar)
In many spinal surgeries, two or more vertebral bones are permanently joined with a technique called “spinal fusion.” A fusion creates a solid mass of bone. It stabilizes your spine.
Superion® InterSpinous Spacer (Vertiflex)
This is an implant that lifts and separates your vertebrae. It’s used to treat lumbar spinal stenosis. That’s a narrowing of the space around your spinal nerves in your lower back. The Superion implant makes more room for these nerves, relieving painful compression.